A Brief Colonial History Of Ceylon(SriLanka)
Sri Lanka: One Island Two Nations
A Brief Colonial History Of Ceylon(SriLanka)
Sri Lanka: One Island Two Nations
(Full Story)
Search This Blog
Back to 500BC.
==========================
Thiranjala Weerasinghe sj.- One Island Two Nations
?????????????????????????????????????????????????Wednesday, April 29, 2020
The COVID-19 pandemic; Why did the world fail to prevent it ?

The world is struggling to survive a viral holocaust. According to the
World Health Organisation, as of 11th April, there were 1,524,161
confirmed cases and 92,941 deaths in 213 countries and territories.
United States, Spain, Italy, Germany, France, China, Iran, United
Kingdom, Turkey and Belgium are the most impacted countries. World over,
the health, economic and social consequences have been profound.
Arguably we could have prevented this pandemic or at a minimum mitigated
its impact. It is important to look at the reasons of our collective
failure to do so, in order to avoid the same mistakes in the future.
According to World Health Organisation 2019 estimates, only 60% of the countries in the world have adequate capacity for early warning, risk reduction and management of national and global health risks, including disease outbreaks
First, COVID-19 just like the Severe Acute Respiratory Syndrome (SARS)
epidemic, most probably originated in the wet markets in China. However,
even after the SARS epidemic which killed nearly 800 people, the world,
collectively failed to regulate/ ban wild life markets which continue
to pose serious global public health risks.
Second, practically all countries are paying the price of inadequate investment in health, particularly surveillance and prevention. Hundreds of doctors and nurses have died in the line of duty. At least some of them could have been saved, if there were adequate personal protective equipment. According to World Health Organisation 2019 estimates, only 60% of the countries in the world have adequate capacity for early warning, risk reduction and management of national and global health risks, including disease outbreaks. Only half of the 194 WHO Member States have reliable death registration systems; so these countries are not even counting the dead accurately.The Covid-19 epidemic has exposed the risk of limiting access to primary care for vulnerable segments of the population, even in high income countries.
Second, practically all countries are paying the price of inadequate investment in health, particularly surveillance and prevention. Hundreds of doctors and nurses have died in the line of duty. At least some of them could have been saved, if there were adequate personal protective equipment. According to World Health Organisation 2019 estimates, only 60% of the countries in the world have adequate capacity for early warning, risk reduction and management of national and global health risks, including disease outbreaks. Only half of the 194 WHO Member States have reliable death registration systems; so these countries are not even counting the dead accurately.The Covid-19 epidemic has exposed the risk of limiting access to primary care for vulnerable segments of the population, even in high income countries.
Third, lack of solidarity between the developed and developing world is
placing the world at risk. Since infectious agents including viruses do
not respect the status of people or borders, poverty, weak health
systems and public health risks in any part of the world are potential
threats to the whole world. The world as a whole and high-income
countries in particular, must recognise that their policies with regard
to development assistance, global health funding, market access for
exports and debt relief in developing countries have an undeniable
impact on global health security.
Fourth reason for failure to prevent pandemic can be attributed to the general lack of accountability of political leaders. Even in countries where they are elected by people, most leaders are more concerned about safeguarding their political future rather than controlling disease outbreaks with well funded, efficient and timely responses. In a few countries the COVID-19 pandemic has even been utilised as an excuse to strengthen authoritarian regimes and get rid of hard working public health officials. Leaders are not held accountable because civil society in most countries is not empowered to demand transparency and accountability from political leadership.
Finally, we have not done enough to strengthen global health governance
to contain the spread of pathogens in an interconnected world.
Regulatory frameworks play a vital role in structuring responses to
major global health challenges like pandemics. At present there is no
clear strategy to share the responsibility of health governance between
local, national, regional and global levels. The 2005 International
Health Regulations (IHR), a collective global agreement about handling
infectious diseases, lacks enforceability mechanisms to respond to
actions of countries that breach IHR obligations.
At least, three universal actions are required to minimise the
likelihood of occurrence of future pandemics. First, National
governments need to increase investment in surveillance systems, public
health and prevention.They need to make health systems accountable to
people through legislation, regulation, transparency, public
participation and education about rights.

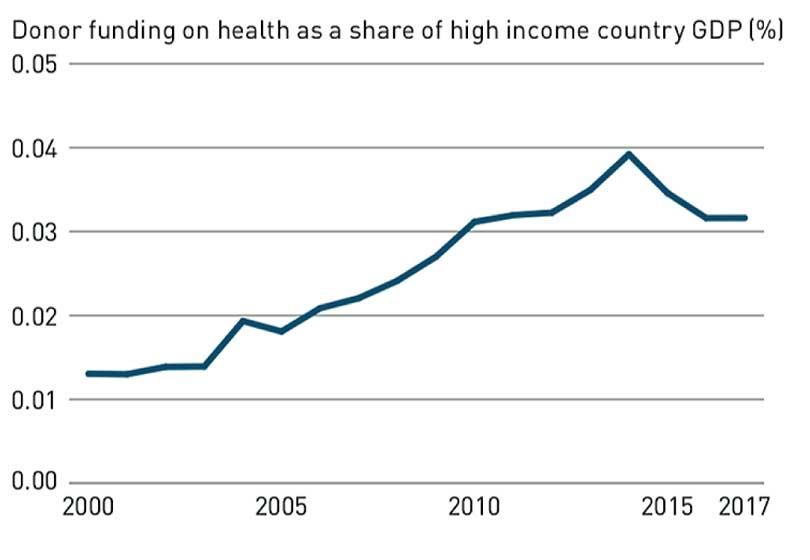
Second, high-income countries should honour their commitments to
development assistance. They should also strongly consider earmarked
funding towards IHR capacity building and compliance, and the creation
of a fund to support research and development for vaccines. Donor
funding for health is still important for many low and low-middle income
countries. However, in 2017, donor funding for health to recipient
countries was just over 0.03% of high income country GDP, and this
fraction has fallen since 2016 (See graph).
Third global health governance and regulatory frameworks such as IHR
need to be strengthened including through strengthening of global
governance institutions for health such as the World Health
Organisation. Wet markets should be banned or controlled so that they do
not continue to be the breeding grounds of virulent pathogens that
threaten the whole world. Civil society needs to be empowered to
motivate political leaders and governments to implement IHR by reporting
their progress to the media, in turn generating reputation-based
incentives.
There is a risk that this pandemic would hinder future global cooperation and create a wave of protectionism. Already at least 69 countries have put in place export restrictions, particularly on masks, gloves, gowns and other personal protective equipment. Some major food producing countries have also imposed restrictions on export of wheat and rice. One hopes that this pandemic will soon prompt a re-examination of the importance of global solidarity. On a positive note, G20 leaders held an emergency virtual summit on the 26th of March and issued a statement on the control of COVID-19. It stated “We will work to ensure the flow of vital medical supplies, critical agricultural products, and other goods and services across borders, and work to resolve disruptions to the global supply chains, to support the health and well-being of all people.” However, the statement failed to spell out clearly its responsibilities in relation to the poorest countries.
There is a risk that this pandemic would hinder future global cooperation and create a wave of protectionism. Already at least 69 countries have put in place export restrictions, particularly on masks, gloves, gowns and other personal protective equipment. Some major food producing countries have also imposed restrictions on export of wheat and rice. One hopes that this pandemic will soon prompt a re-examination of the importance of global solidarity. On a positive note, G20 leaders held an emergency virtual summit on the 26th of March and issued a statement on the control of COVID-19. It stated “We will work to ensure the flow of vital medical supplies, critical agricultural products, and other goods and services across borders, and work to resolve disruptions to the global supply chains, to support the health and well-being of all people.” However, the statement failed to spell out clearly its responsibilities in relation to the poorest countries.

Uncontrolled wet markets selling snakes, dogs, cats, bats and exotic animals are breeding grounds for virulent pathogens
We will survive this pandemic just as we survived the influenza pandemic
H1N1 (2009), SARS (2003), Middle East Respiratory Syndrome Coronavirus
(MERS) (2013), Ebola crisis (2014) and the Zika virus (2016). However,
it would be at a much greater cost to human lives and the global
economy. The image of people and health workers dying in horrific
numbers even in the richest and most powerful countries should leave an
indelible mark on the world’s collective conscience. When this pandemic
is under control, we owe it to future generations to seize the
opportunity to transform national and global responses to epidemics. The
next pathogen that emerges, may be too virulent to give mankind yet
another chance for survival.
The writer was Former Senior Adviser, World Health Organisation, Geneva,
Switzerland for 20 years and former Professor of Medicine, Faculty of
Medicine, Peradeniya